Accuracy of the 6 Most Common Parasite Tests
There are 6 commonly used parasite tests. By comparing all 6, I think it’s clear that 1 parasite test that is most accurate for diagnosing parasitic infections.
Here are the 4 things you want to look for when evaluating your parasite test:
- How many species of parasites can it diagnose?
- How accurate is the test?
- Can the test tell the difference between an old parasite infection and a current infection?
- How convenient is taking the test?
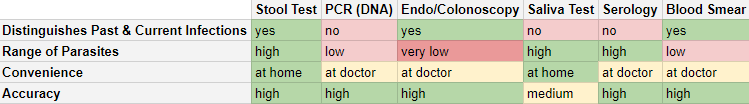
Quick facts about the most common parasite tests:
- For almost everyone in the USA, the ova and parasite stool test will look for over 31 intestinal parasites, with the highest accuracy.
- The DNA database for PCR parasite testing is quite small. Only 5-9 gut parasites parasites can be found with commercially available testing.
- Blood and saliva antibody parasites tests don’t reliably distinguish between current and past infections, and are most useful in niche situations.
- Colonoscopies are not reliable parasite tests because they can’t find common microscopic parasites, and may miss even larger worm parasites.
Ranking of the 6 Best Parasite Tests
Now we’ll go through each of the 6 tests – ranking them from worst to best:
- Fecal Exam aka Ova & Parasite testing
- PCR (Parasite DNA) Testing
- Saliva Test
- Serology Blood Test
- Blood Smear
- Endoscopy/Colonoscopy
1. Fecal Exam AKA Ova & Parasite testing
This test, also known as microscopy, takes some feces, processes it, concentrates it, stains it, and then places it onto a microscope slide.
The technician then looks at the feces through a microscope and visually inspects and records what parasites, and parasite eggs (called ova) they observe.
In our high-tech world, this “manual” method of parasite detection seems out of place. But when it comes to real-world parasite infections, this is typically the most effective and reliable test for the following reasons:
- Samples are collected over 3-8 days – making it unlikely that the parasites will be missed while the parasite spends part of its life cycle outside of the intestines in other organs…or the parasite may be stressed and not laying eggs.
- Experienced technicians can identify a huge range of parasites that PCR and antibody/antigen tests can’t identify. 30+ parasites can be identified by the best-trained Ph.D. Parasitologists, but only 5+ parasites can be identified by DNA PCR methods.
- The severity of the infection can be judged by an experienced technician more reliably compared to PCR (which may over-amplify minor infections)
- This test doesn’t confuse prior infections, with current infections (unlike PCR and antibody tests). If the test is negative for parasites, and symptoms are gone, then it’s very likely that the parasite has been removed.
What does a positive test mean for you?
When performed correctly, a positive test means you DO have a parasite infection. The range is wide, and it can tell you about a wide range of possible infections you could have – even microscopic infections.
What does a negative test mean for you?
This is a fairly accurate test. It could miss a mild infection but, because the specimen Is concentrated, stained, and microscopically examined, the “miss rate” is very low…assuming the lab technician or parasitologist is well trained and experienced.
- Learn how the stool ova and parasite test works
- Learn about our accurate at-home ova and parasite stool test.
2. PCR – Parasite DNA Testing
This test is quite amazing and can give testing results very quickly (as fast as 24 hours). Essentially the technician takes the stool sample, puts it into a machine, and tells you which parasite DNA it has found.
According to my teacher Emma Lane of Integrative Health in the UK, PCR has a strong future in parasite testing. But, she also says that it isn’t the ideal way to test for parasites today.
There are serious drawbacks to using PCR technology in its current state:
- The number of detectable parasites is small. In researching PCR parasite tests, I couldn’t find a DNA parasite analysis that found more than 8 parasites with PCR. While these are some of the most common parasites, there is a much wider range of parasites that infect people, and people who can have exotic parasites due to travel, or contact with immigrants.
- In the sales document of a PCR testing machine, the company says: It is important to remember that…only those organisms that are designated and tested for can be detected. This is especially important when patients have been overseas. An even greater range of infectious organisms may be present in those who are immigrants, refugees, or those who are immunocompromised…
- DNA is detectable from current infections, and infections from the recent past, even if you were treated. So, PCR testing is not effective for determining if your infection is current or a resolved past infection
What does a positive test mean for you?
PCR tests are very sensitive in detecting parasites, but they do not help you decide if the symptoms you have now are from the parasite the test detects. Recently treated infections will still be positive for parasite DNA.
What does a negative test mean for you?
The range of parasites detected with PCR testing is too small. A negative test does not mean you do not have a parasite the test is not able to pick up on.
3. Serology Blood Test + 4. Saliva Test
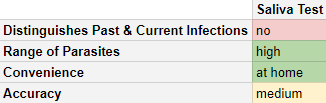
In this test, blood is drawn (or saliva is collected) and then tested for antigens and antibodies that are specific to certain parasites. While this is a relatively painless procedure, it has some serious drawbacks.
Here are the drawbacks:
- If you ever get infected by a parasite, you’ll have antibodies in your body for life. So, a positive IgG test could mean you had an infection a decade ago and your body fought it off. Or, it could mean you are currently infected with parasites. Unfortunately, these tests are almost useless for knowing if you’ve beat the infection after treatment.
- If your lab can test for IgM antibodies, and you come back positive for high enough IgM antibodies, then that would be an indication of a current infection. But you have to be tested for this antibodies at the exact window for when these are produced, which may not be right when you’re exposed, but a bit after that. And if you test for IgM outside of that window, you may only find other antibodies, making it inconclusive if you’re currently infected or not.
- The blood tests only look for specific species. For example, 3 parasite species of the genus Schistosomiasis may cause urinary issues. If your doctor’s test kit only tests for 2 of the 3, then you could have a parasite infection but have a negative serology test.
Blood Parasite Test vs. Saliva Test
Saliva has only one of several types of antibodies you make when you have an infection. This means that the quantity of antibodies is less in saliva, which makes many antibody-based saliva tests far less sensitive than blood testing for antibodies to parasites. That could mean that you had or are infected by a parasite, but your saliva may not show that.
The saliva test is convenient, but it has the same limitations as the blood test. Worse still, since saliva has just one type of antibody, it may show you aren’t infected with a parasite, even if you currently are infected.
What does a positive saliva/blood serology test mean for you?
Both blood and saliva testing are good at saying you have once had an infection. They are terrible, however, at telling you if you just got infected or had an infection in the past.
What does a negative saliva/blood serology test mean for you?
Blood tests will be fairly accurate in saying you never had a parasite infection if the test is negative. Saliva tests are less accurate. On the other hand, if you got infected in the last few days, you will not have built up antibodies to fight that parasite infection, so the test can also be negative when you DO have an infection.
- Read our in-depth article about blood serology antibody tests
- Learn more about different ways to test blood for parasites
5. Blood Smear
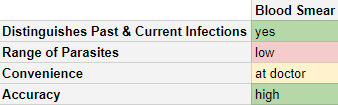
The blood smear tests are very important for diagnosing blood-borne parasites. With the rise of Lyme disease in the USA, Babesia is a blood parasite coinfection of Lyme disease. There are other rare USA blood parasites, but I would not bet on being infected by them…even if a blood smear can find USA blood parasites like Trypanosoma cruzi (causing Chagas disease).
A blood smear parasite test may be vital if you’ve fallen ill after spending time in a place with blood-borne parasites (like malaria).
Overall, the accuracy of this test is very high (assuming the technicians are competent), but the range of parasites is too limited for it to be useful for most people reading this website [one notable exception could be if Lyme disease is suspected]. Therefore I would not rate this as useful for most people. Be sure to refer to the CDC website to see if you’re traveling to a place that is endemic with blood-borne parasites.
What does a positive test mean for you?
It means you DO have a parasite that shows up in the blood. Most parasites, however, DO NOT show up on a blood smear.
What does a negative test mean for you?
It doesn’t mean much. You could still have one of many parasites that can’t be detected in a blood smear, or the technician may not be well trained or experienced.
6. Endoscopy/Colonoscopy Parasite Test
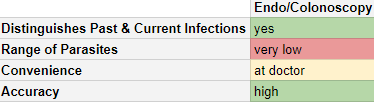
What is an Endoscopy/Colonoscopy?
An endoscopy/colonoscopy involves sticking a small camera down your throat or up through your colon. Your gastroenterologist can look at a live video of your colon, or your stomach and small intestine.
How Can an Endoscopy/Colonoscopy Diagnose a Parasite Infection?
If your doctor spots a parasitic worm (helminth) in your intestines, then your doctor can diagnose a parasite infection.
How does this parasite lab test rate on the 4 criteria?
Range of parasites:
Your doctor can only see large parasites with this method of diagnosis. Many species of parasites are microscopic and can’t be seen without magnification. Parasite eggs are a reliable way to diagnose worm infections. But eggs need up to 1000x magnification, which is not achievable with endoscopy tests.
Accuracy:
If your doctor can visually see a parasite wriggling around in your intestines, then you definitely have a parasite infection. If the doctor misses the worm, you might have a false negative test, even for the few large parasites detectable by this test.
What does a positive test mean for you?
A positive test usually means you DO have a species of worm. Worms are only one of a much greater variety of parasites, so it doesn’t mean much in the greater span of parasite infections.
What does a negative test mean for you?
A negative test is almost meaningless. It could easily mean you DO have a parasite, but the test did not detect it.
Differentiating Old and New Infections:
Your doctor will only be able to see current infections.
Convenience:
A colonoscopy/endoscopy can only be performed with special equipment in a doctor’s office. Additionally, patients have to undergo uncomfortable bowel prep by taking a strong laxative.
I would personally not rely on a colonoscopy or endoscopy for a complete diagnosis of parasite infections. Many parasites are invisible without staining and magnification, so it won’t reliably diagnose parasites except the largest ones.
- Click here to read our more in-depth analysis of the endoscopy/colonoscopy parasite test.
Conclusions About The Best Parasite Test
In summary, here’s how I would rate each of the tests:
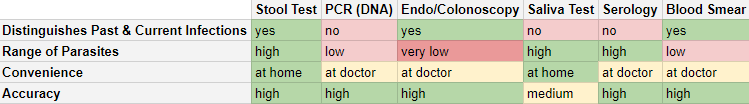
Unless you’ve been traveling to a place that has malaria or other blood-borne parasitic diseases, the stool test (Parasite and Ova) stool test is typically the best.
If the lab tech is skilled and experienced, the parasite and ova test:
- Can diagnose a huge number of human-infecting parasites
- Can be taken in the comfort of your own home
- Won’t confuse past and current infections
- Is extremely accurate
Click here to learn about our highly accurate home parasite stool test kit
Article sources:
1. Khan MQ, Gentile N, Zhou Y, Smith BA, Thomson RB, Yen EF. An audit of inpatient stool ova and parasite (O&P) testing in a multi-hospital health system. J Community Hosp Intern Med Perspect. 2020;10(3):204-209. Published 2020 Jun 14. doi:10.1080/20009666.2020.1760422.
2. John A. Branda, Tai-Yuan David Lin, Eric S. Rosenberg, Elkan F. Halpern, Mary Jane Ferraro, A Rational Approach to the Stool Ova and Parasite Examination, Clinical Infectious Diseases, Volume 42, Issue 7, 1 April 2006, Pages 972–978, https://doi.org/10.1086/500937.
3. A Case of Parasite Invasion of the Intestinal Tract: A Missed Diagnosis in Irritable Bowel Syndrome. Clin Endosc. 2013;46 (6): 671-674.
4. Alessandra Ricciardi, Momar Ndao. Diagnosis of Parasitic Infections: What’s Going On? Journal of Biomolecular Screening, Volume: 20 issue: 1, page(s): 6-21. Article first published online: August 28, 2014.
5. Sow D, Parola P, Sylla K, et al. Performance of Real-Time Polymerase Chain Reaction Assays for the Detection of 20 Gastrointestinal Parasites in Clinical Samples from Senegal. Am J Trop Med Hyg. 2017;97(1):173-182. doi:10.4269/ajtmh.16-0781.
6. Jon E. Rosenblatt, L. Barth Reller, Melvin P. Weinstein, Laboratory Diagnosis of Infections Due to Blood and Tissue Parasites, Clinical Infectious Diseases, Volume 49, Issue 7, 1 October 2009, Pages 1103–1108, https://doi.org/10.1086/605574.
7. Ndao M. Diagnosis of parasitic diseases: old and new approaches. Interdiscip Perspect Infect Dis. 2009;2009:278246. doi:10.1155/2009/278246.
Additional Article sources:
- CDC references on diagnosing parasite infections.
- CDC article on detecting parasites via antibodies.
- Human saliva as a source of anti-malarial antibodies to examine population exposure to Plasmodium falciparum
- PCR Testing: Advantages, Limitations and Interpreting Results, County of Monterey
